NIV vs HFT Quiz
Which therapy would you use for a chronic obstructive pulmonary disease patient with

NIV vs HFT Quiz
Play video and select an answer
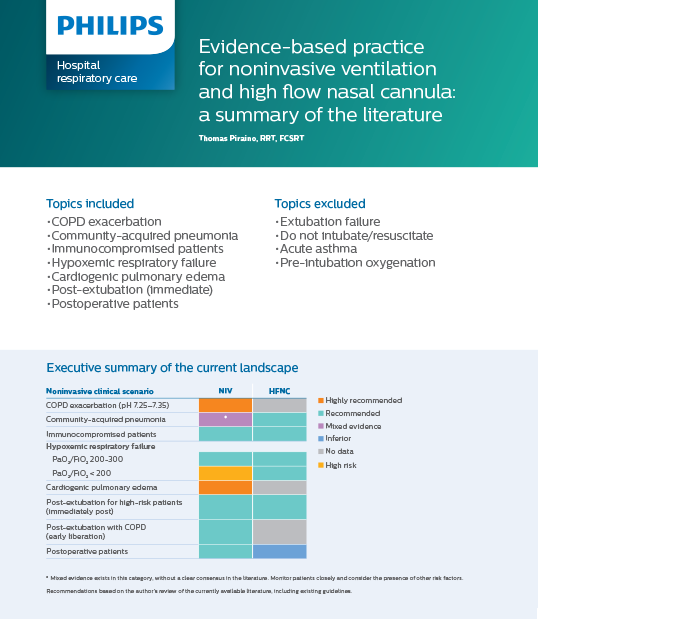
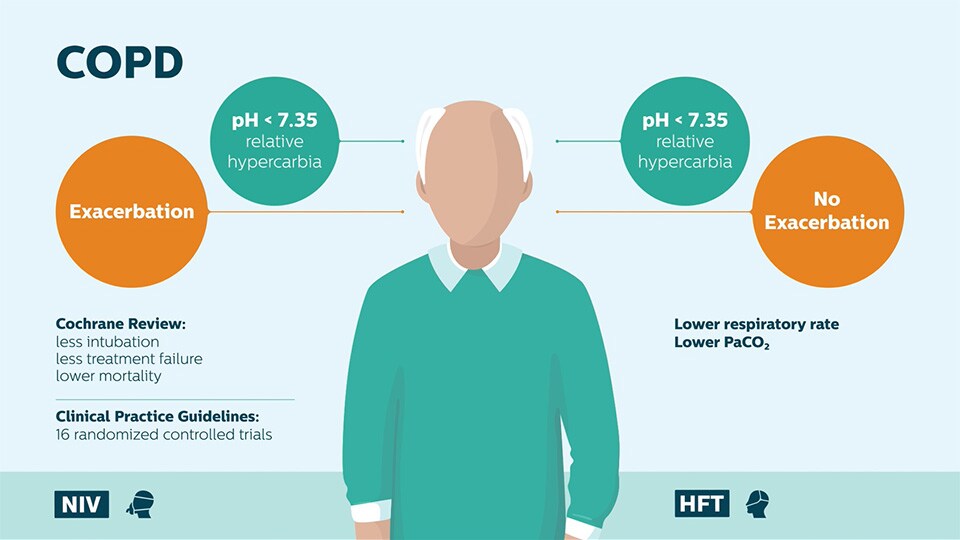
Which therapy would you use for a COPD patient with exacerbration?
NIV vs HFT Quiz
Answer
NIV vs HFT Quiz
Play video and select an answer
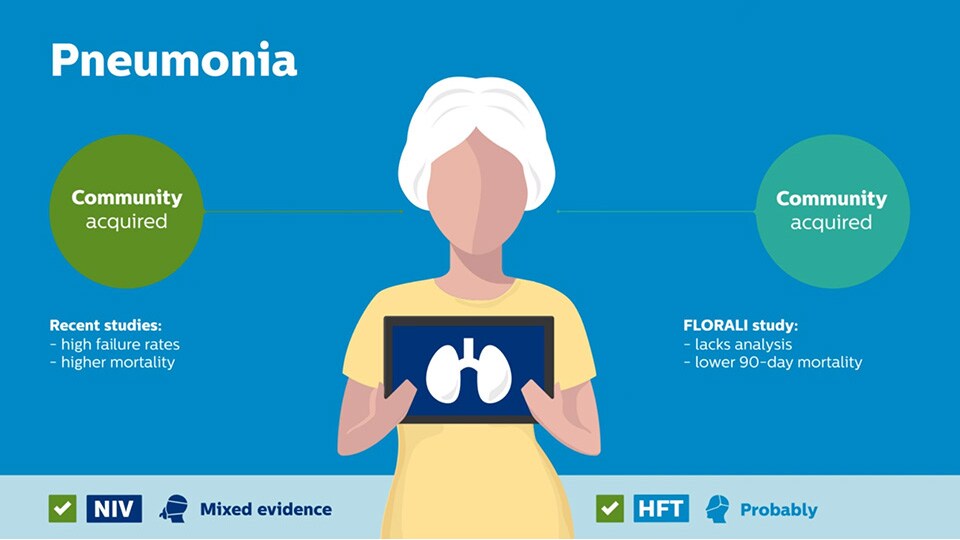
Which therapy would you use for a COPD patient with community-acquired pneumonia?
NIV vs HFT Quiz
Answer
NIV vs HFT Quiz
Play video and select an answer
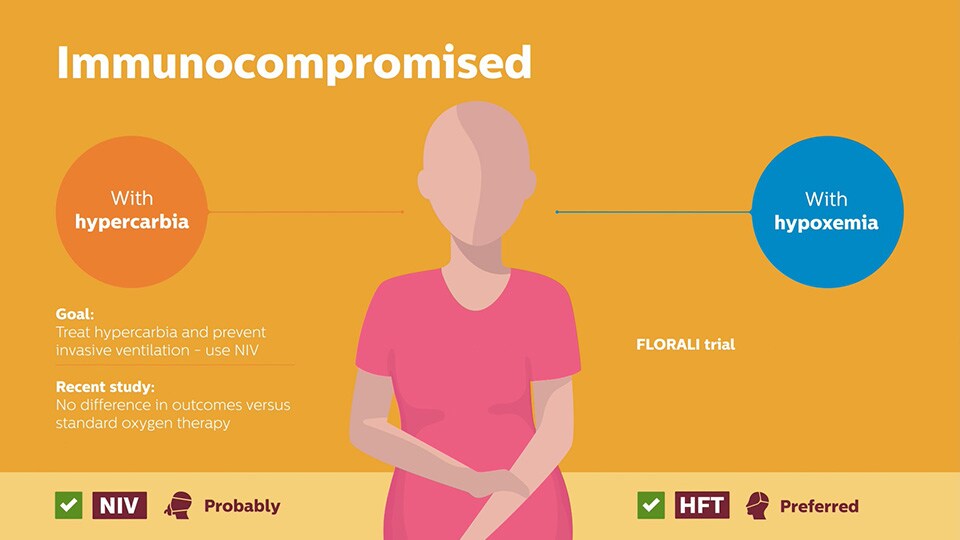
Which therapy would you use for a Immunocompromised patient?
NIV vs HFT Quiz
Answer
NIV vs HFT Quiz
Play video and select an answer
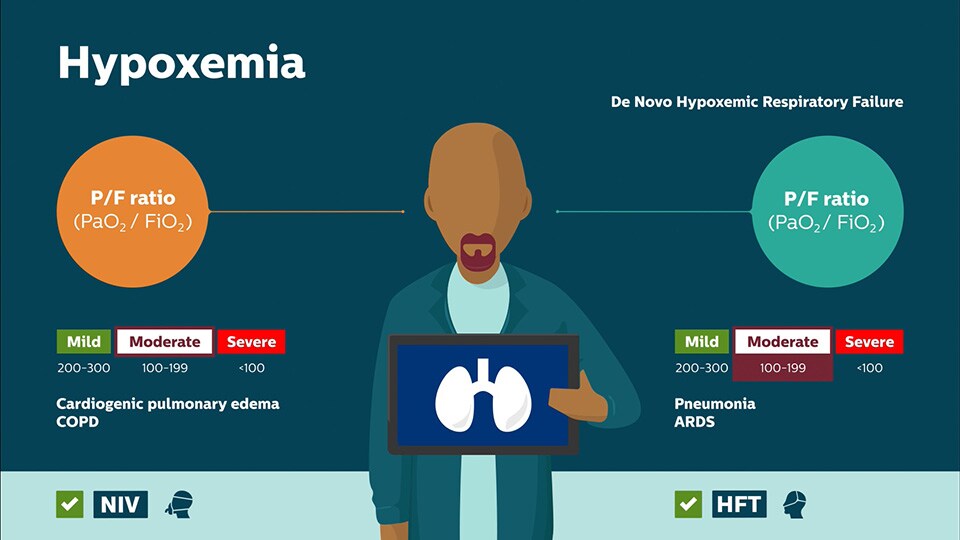
Which therapy would you use when treating a hypoxemic?
NIV vs HFT Quiz
Answer
NIV vs HFT Quiz
Play video and select an answer
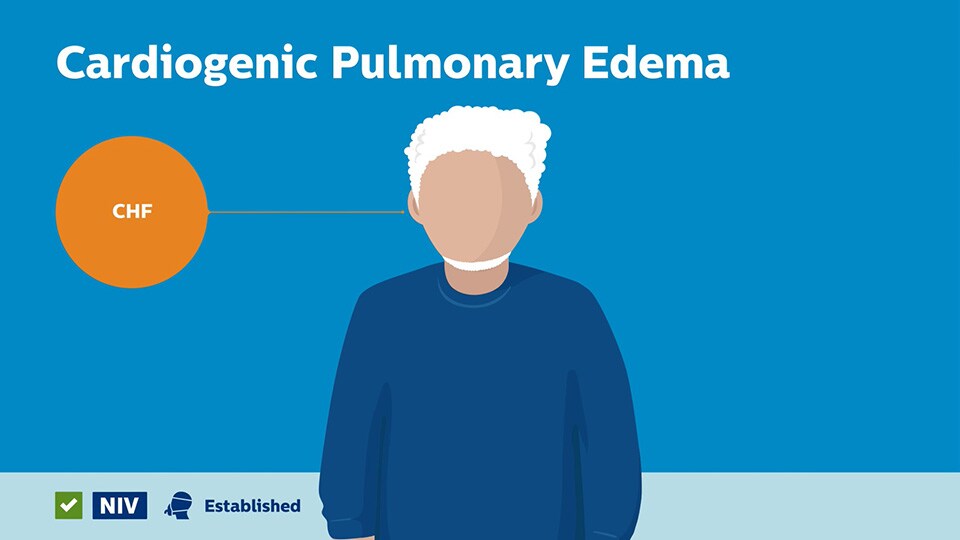
Which therapy would you use when managing a cardiogenic pulmonary edema patient?
NIV vs HFT Quiz
Answer
NIV vs HFT Quiz
Play video and select an answer
Which therapy would you use when treating a post-extubation patient?
NIV vs HFT Quiz
Answer
NIV vs HFT Quiz
Play video and select an answer
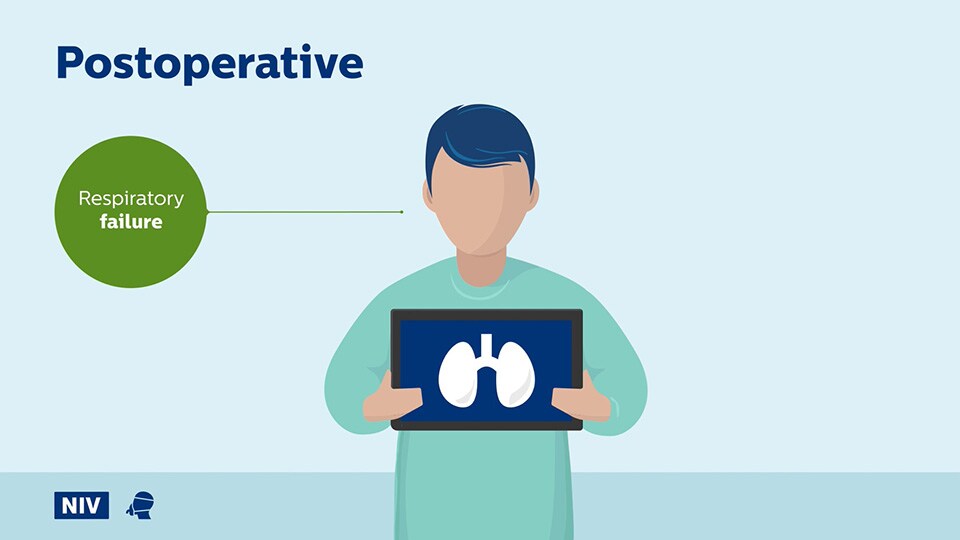
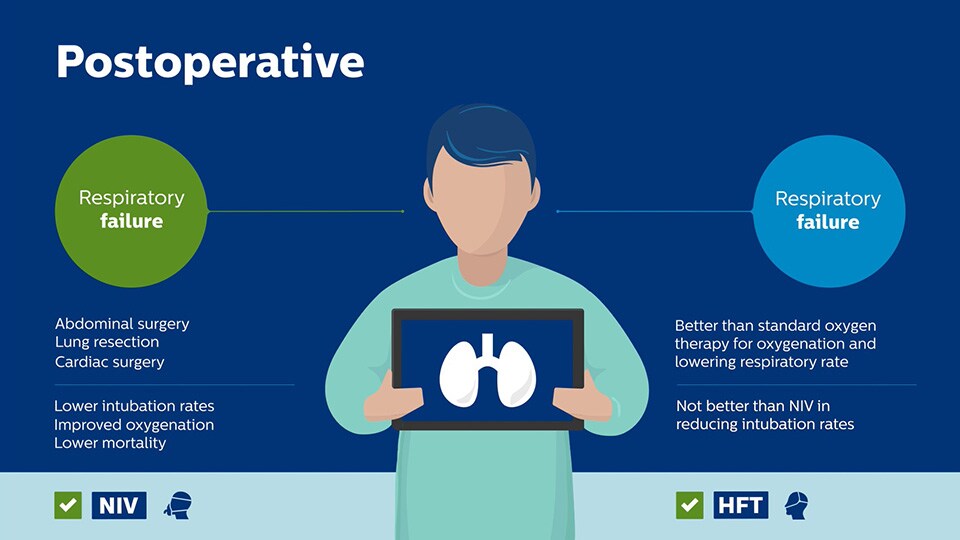
Which therapy would you use when managing a postoperative abdominal patient?
NIV vs HFT Quiz
Answer
NIV vs HFT Quiz