FieldStrength MRI magazine
User experiences - April 2015
Beaumont Health System brought MRI into its radiation therapy routine practice by implementing the comprehensive Ingenia 3.0T MR-RT Oncology Configuration.
The potential benefits of using MR in radiation therapy planning are obvious: with its excellent soft tissue contrast, MR images can help to define lesions for well-targeted radiation therapy (RT) planning. During treatment, MR can visualize changes in patient anatomy and tumor biology to help adapt the treatment plan to these changes. Post-treatment MRI is used to monitor treatment response.
“The superb soft tissue contrast allows detailed delineation of tumors and healthy organs, which is crucial for RT planning.”

Di Yan, D.Sc., FAAPM
Di Yan, D.Sc., FAAPM is Chief Physicist, Radiation Oncology, Beaumont Health System and Professor, Oakland University William Beaumont School of Medicine. His current research interests include image guided/adaptive radiotherapy, treatment response assessment and outcome modeling, and motion management, dynamic delivery and simultaneous imaging.

Craig W. Stevens MD, PhD
Craig W. Stevens MD, PhD is the System Chair of Radiation Oncology for the Beaumont Health System. He is the former Chair of Radiation Oncology at the Moffitt Cancer Center in Tampa, and was a Professor in the Department of Oncologic Sciences at the University of South Florida. He earned his PhD in Cancer Biology, and his MD from Northwestern University after a BS in Biology from MIT.
MRI integrated in radiation oncology department
Beaumont Health System (Royal Oak, Michigan, USA) is one of the largest health systems in the USA, with eight hospitals and 153 outpatient sites, a medical school and a research institute. The Radiation Oncology (RO) department houses a dedicated Ingenia MR-RT solution that is routinely used for clinical and research MR-RT activities. “The main reason to integrate MR imaging in RT planning is the superb soft tissue contrast that allows detailed delineation of tumors and healthy organs, which is crucial for RT planning,” says Craig W. Stevens MD, PhD. “MR also provides information on functional and biological activities in tumors, background tissue and normal organs, which may also be used in RT planning,” says physicist Di Yan, DSc, FAAPM.” “We currently use MR-RT mainly in the abdomen and pelvis region: prostate, colorectal, pancreatic, cervical, and liver. Also in the brain, we are starting to use it,” says Dr. Yan.
“The good visualization is why a lot of cancer treatments can benefit from MR based treatment planning, because if we can localize a tumor better, we can aim the radiation beam at it better. This potentially allows us to shrink our margins and spare more healthy tissue.”

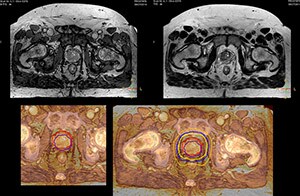
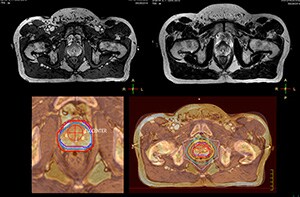
Impressive clinical benefits for prostate
“The biggest problem for CT-based planning, especially in prostate, is you can’t see the cancer very well,” says Dr. Stevens. “On CT it can be quite challenging to see the edge of the prostate especially at the apex. When the edge of the prostate can’t be delineated well on CT, radiation oncologists will increase their margins a little bit so they don’t miss it, but that can also increase toxicity.” “Using MR, the prostate is well delineated. We quickly see the edges of cancerous tumors like in prostate cancer, and as normal structures can be defined, we can optimize the treatment plan to protect these organs and their normal function. This can potentially improve the outcome. And it improves workflow as well. We can contour more quickly, confident that the tumor is going to be in the field.” “The Ingenia 3.0T MR scanner provides high resolution allowing us to make scans fast for the patients. It also gives the potential to include methods like MR spectroscopy and diffusion weighted Imaging, which we’re in the process of doing right now,” Dr. Stevens adds.
Special requirements for MRI in RT planning
“There are some general challenges in RT imaging – even with CT – such as imaging geometry and positioning accuracy. Positioning is extremely important in RT, because we need reproducibility between imaging and treatment position. We also need accurate geometry so we can be sure our treatment plan is properly delivered during the treatment,” says Dr Yan. “The Ingenia MR-RT configuration includes an external laser positioning system for patient alignment and a flat tabletop for imaging the patient in treatment position. Ingenia MR-RT also came with a special QA package for regular monitoring of precision. Our Ingenia 3.0T scanner achieves good geometric accuracy – within a millimeter for most patients – and the phantom measurement is even better,” he adds. “Ingenia’s wide 70 cm bore is valuable to easily accommodate immobilization devices needed in RT,” says Dr. Stevens. “With a small bore MR scanner you can’t get the RT immobilization devices into the scanner properly; the large bore makes it easy to image patients in their immobilization device.”

The potential benefits of using MR in radiation therapy planning are obvious: with its excellent soft tissue contrast, MR images can help to define lesions for well-targeted radiation therapy (RT) planning. During treatment, MR can visualize changes in patient anatomy and tumor biology to help adapt the treatment plan to these changes. Post-treatment MRI is used to monitor treatment response.
“A lot of cancer treatments can benefit from MR based treatment planning, because if we can localize a tumor better, we can aim the radiation beam at it better.”
Implementing MR-RT in the department
“When a patient registers, first CT simulation and MR simulation are done, followed by CT-MR registration on Pinnacle3. Then the target and normal organ delineation is performed on MR images. Meanwhile we create a reference CT image for online treatment and localization correction. During the treatment phase we can perform additional MRI scans to visualize the anatomy changes and create an adaptive plan. This plan basically adapts the treatment plan to the changes.” “Along with its great benefits, MR has introduced some new challenges,” Dr. Stevens says. “Radiation therapy teams generally have no experience with MR. The Philips training helped us to implement fully the things we can do with the Ingenia MR-RT system. So the training, as well as having a good MR physicist, is critical.”
“Our staff was quite ready to take on the new way of working with MR-RT. After MR-RT was introduced, most of our clinicians said it made their lives easier,” says Dr. Yan.
MR imaging for brain treatment planning
“Also in brain tumor treatment planning the MRI soft tissue contrast offers a great advantage for seeing the target boundary. Brain tumors often involve edema, and CT cannot show this. Besides, MR also provides diffusion and perfusion information on background tissue,” says Dr. Yan. “MR is a powerful method for imaging brain tumors. I think we should never treat a brain tumor without having good MR imaging we can trust,” Dr. Stevens says.
Future outlook
“I think that in the future functional information from MRI is going to become much more important, both for prognostic and predictive measures, as well as for treatment response measures,” Dr. Stevens concludes. “With Ingenia MR-RT we will have the ability in our department to make decisions based on, for instance, changes in blood flow and diffusion at the beginning, middle and end of treatment. I believe that over time, every large cancer center will need to have an MR scanner in their radiation oncology department.”
Results from case studies are not predictive of results in other cases. Results in other cases may vary. Results obtained by the facility described in this article may not be typical for all facilities.
“The large bore makes it easy to image patients in their immobilization device.”