velj 17, 2022 by Philips
Reading time: 9-10 minutes
The power of MRI and MRI/US biopsy to aid in prostate cancer diagnosis

An alternative patient pathway for prostate cancer diagnosis
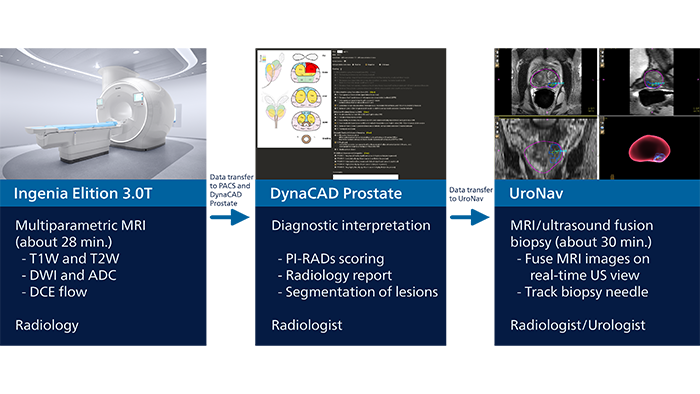
Moving from TRUS biopsies to multiparametric MRI and targeted biopsies guided by fused MRI/ultrasound images is benefiting high-risk prostate cancer patients at WellSpan York Hospital in York, Pennsylvania. Dr. Edward Steiner has collaborated with urologists to set up an alternative patient pathway for prostate carcinoma diagnosis through the use of multiparametric MRI and MRI/ultrasound fusion for targeted biopsies. Particularly when a patient with clinically significant prostate carcinoma has had multiple negative TRUS biopsies before, this targeted procedure can assist urologists to quickly make a confident diagnosis, and allows patients to start therapy as soon as possible. This may be life-changing for the patient.
The value of multiparametric MR imaging
The use of MRI has significantly improved capabilities in prostate cancer diagnosis, according to Dr. Steiner. “Multiparametric prostate MRI allows us to look at three parameters to build our diagnosis on: conventional T1 and T2 signal intensity, diffusion-weighted imaging and ADC map, as well as dynamic flow imaging, to define the highest probability of prostate carcinoma.” The standard PI-RADS1 system is then used to grade lesions based on the MRI findings. For PI-RADS 1 and 2, clinically significant cancer is (highly) unlikely. Intermediate PI-RADS 3 lesions represent a kind of diagnostic “gray area” – these lesions may become PI-RADS 4 lesions if they demonstrate a hypervascular tumor flow pattern or depending upon index of suspicion. PI-RADS 4 and 5 lesions have a statistically high chance of being a clinically significant prostate carcinoma and should be biopsied. Once biopsy is performed, the pathologists characterize the biopsy samples with either a Gleason score or an ISUP grade group.2 “Contrary to other techniques, MRI allows for examination of the entire prostate gland with high soft-tissue contrast,” says Dr. Steiner. “Multiparametric MRI allows us to identify suspicious lesions and give these a PI-RADS score. For high-risk lesions, a biopsy can then be performed, guided by MRI images that are fused with ultrasound images in real time. This allows targeting of the lesions that were identified before.”
The power of multiparametric MRI is now not only recognized for exams to identify suspicious lesions, but also expands into guiding biopsies to inform a definite diagnosis.”
Edward Steiner, MD, FACR
Chief and Medical Director at WellSpan Advanced Prostate Care Center
Predictable MRI patterns help identify suspicious lesions
Depending upon the Gleason score and prior therapies, prostate carcinoma has a certain predictable pattern on multiparametric MRI, according to Dr. Steiner. “In general, lesions in the peripheral zone have decreased T2-weighted signal and are relatively focal,” he says. “In the transitional zone, these lesions are more difficult to evaluate on T1 and T2, but are generally non-encapsulated.”
“We also look at diffusion-weighted images and the ADC map. Prostate neoplasms generally have diffusion restriction, so they are bright on diffusion-weighted imaging and dark on an ADC map, which is one of the most important characteristics of neoplasms.”
“The third characteristic we look at, flow, is somewhat less specific but may be quite important in deciding whether a lesion is significant or insignificant. Prostate neoplasms often have a hypervascular tumor flow pattern, meaning that there is rapid inflow of blood into the lesion and then rapid outflow due to a disrupted capillary bed. This can be graphed on multi-parametric images, allowing us to define regions of interest and look at the actual flow within these regions.”
“I perform this interrogation using DynaCAD prostate, which also provides an easy way to determine PI-RADS score and create the report for the urologist.”
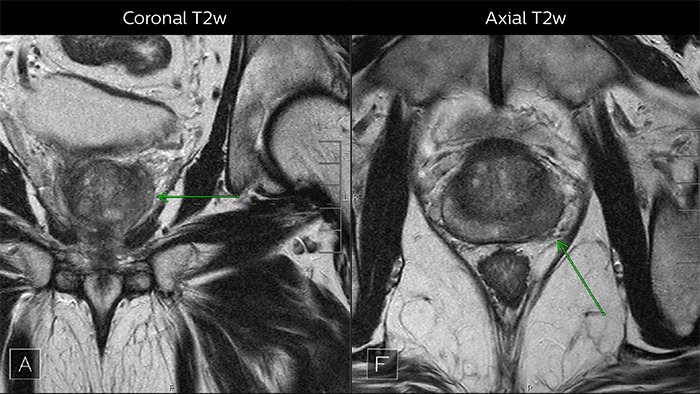
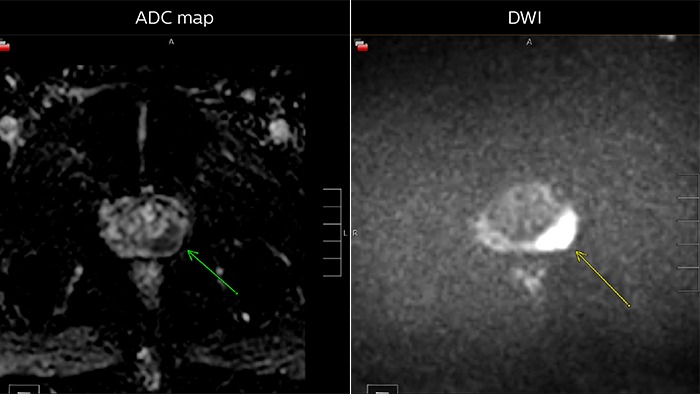
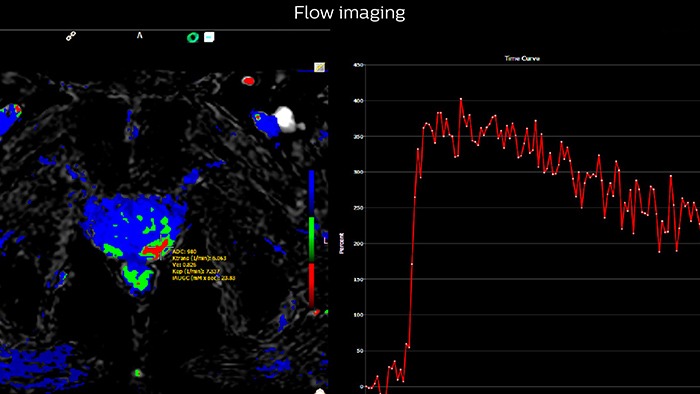
Multiparametric MRI of a classic peripheral zone lesion Dr. Steiner describes this case: “For lesions in the peripheral zone of the prostate, the DWI (diffusion weighted imaging) and ADC map are most helpful for diagnosis. In this case, the DWI shows a very bright signal, which indicates diffusion restriction. The arcuate area with significant signal drop out (arrow) on the ADC map is recognized as highly suspect for tumor. On the axial T2-weighted image the capsule contour looks a little irregular (arrow), which we interpret as capsular disruption, and I usually give a measurement: this lesion shows larger than 1.5 cm capsular disruption. I don’t see any signs of lymphadenopathy, but interpret this lesion as PI-RADS 5. The hypervascular flow pattern in the bottom images adds to the diagnostic confidence.”
Using detailed, segmented MRI images to guide prostate biopsy
Dr. Steiner explains how a “blind” ultrasound biopsy may lead to a negative result, even when a tumor is present. “In a non-targeted biopsy guided by ultrasound, you see the needle and the confines of the prostate, but cannot see the tumor. So, when trying to get 12 cores as evenly distributed as possible, the tumor may still be missed, particularly when it is in the anterior gland, low in the apex or in other regions generally not easily biopsied by ultrasound.” This is why Dr. Steiner has implemented a pathway where the MRI images can also be used to guide the biopsy. He uses an MR/ultrasound fusion guided biopsy device, UroNav, which fuses pre-biopsy MRI images of the prostate with real-time ultrasound images during transrectal biopsy, for excellent delineation of the prostate and suspicious lesions, as well as clear visualization of the biopsy needle path. “I felt strongly that urologists are used to doing free-hand biopsies – their brain and hand are very used to manipulating the probe,” says Dr. Steiner. “What UroNav offers is no change in that workflow; it takes the diagnostic MRI images and the localized, segmented lesions and adds tracking and navigation to fuse that with the live ultrasound images. In this way, the MRI images can be used for targeting the lesion when performing the biopsy. The UroNav navigation sensor is mounted on the TRUS probe*, so for urologists the manipulation is similar to what they were used to.” “This process allows us to perform focal biopsies of suspicious areas based on PI-RADS categories that indicate the probability of an underlying potential malignancy,” says Dr. Steiner.
Early experiences
“I partnered with one of our local urology groups and we jointly did the first ten MRI fusion biopsies in our operating room, which gave us both experience as well as leadership. Having the UroNav capability added ‘GPS navigation’ to the urologist’s normal workflow and we could perform targeted biopsy. And I already owned DynaCAD, from which data could directly be imported to UroNav. It was a great win-win,” Dr. Steiner says.
“DynaCAD allows me to easily import the images into UroNav for eventual biopsy,” he says. “The decision for biopsy is taken after interpreting the MRI. So, if I don’t use DynaCAD/UroNav I would have to import the data into another modality and literally need to redo all of my work.”
The alternative patient pathway for prostate cancer diagnosis
“In our first 13 cases of repeat fusion biopsy following negative TRUS biopsy, 11 patients yielded positive tissue for clinically significant carcinoma; 92% of 48 targeted cores were positive in PI-RADS 4 and 5 lesions. The entire procedure takes less than 20 to 30 minutes, and patients who have previously experienced a conventional transrectal ultrasound-guided biopsy often remark on how easy this procedure is.”
Edward Steiner, MD, FACR
Chief and Medical Director at WellSpan Advanced Prostate Care Center
Conclusion
Dr. Steiner emphasizes that the power of MRI is now recognized not only for multiparametric examinations to identify suspicious lesions, but also expands into guiding biopsies to inform a definitive diagnosis.
“Patients that have PI-RADS 4 and 5 lesions on MRI have a high risk for clinically significant carcinoma. Such lesions are often in the anterior gland, low in the apex, or near regions generally not easily biopsied by ultrasound. These patients now receive MRI/ultrasound fusion biopsies, and this has been our standard of practice now for a year,” says Dr. Steiner. “In my opinion, the combination of MRI and ultrasound fusion biopsy is extremely powerful. We will be doing more and more of these biopsies and scans for the future.”
Explore our prostate products and capabilities
-
UroNav
UroNav fuses pre-biopsy MR images of the prostate with ultrasound-guided biopsy images in real time, for excellent delineation of the prostate and suspicious lesions, as well as clear visualization of the biopsy needle path. Combining electromagnetic tracking and navigation with an onboard computer and a real-time imaging interface, UroNav brings precision targeting to your clinical practice in one easy-to-use, mobile workstation.
784026 -
DynaCAD Prostate
Offers a comprehensive set of tools for real-time analysis, review, and reporting of multi-parametric, multi-vendor(3) MRI studies. Enhances productivity by transferring images directly from the MRI to DynaCAD and utilizing its robust, automatic post-processing tools and display the results in customized hanging protocols for analysis and reporting.
784029 -
Ingenia Elition 3.0T X
The Philips Ingenia Elition solution offers cutting-edge MR imaging techniques, while setting new standards for clinical research in 3.0T imaging based on gradient- and RF designs. The Ingenia Elition delivers on superb image quality, and performs MRI exams up to 50% faster¹. Fast overall exam-time is achieved by improving patient handling setup time at the bore with the touchless guided patient setup, combined with accelerations in both 2D- and 3D scanning. Furthermore, the Ingenia Elition offers an immersive audio-visual experience to calm patients and guide them through MR exams.
781358
Share this article
Sign up to receive news and updates from Philips

Edward Steiner, MD, FACR Chief and Medical Director WellSpan Advanced Prostate Care Center York, Pennsylvania, USA
Explore more
References *Contact Philips to ascertain compatibility with your system. 1. Prostate Imaging Reporting & Data System - PI-RADS 2015 version2. ACR American College of Radiology. 2. Van Loenhout R, Zijta F, Smithuis R, Schoots I. Prostate Cancer - PI-RADS v2. Radiology Assistant, https://radiologyassistant.nl/abdomen/prostate-cancer-pi-rads-v2 PI-RADS® is a registered trademark of The American College of Radiology. Results from case studies are not predictive of results in other cases. Results in other cases may vary.






